Arthritis of the Thumb
Introduction
Physiotherapy in Edmonton for Hand
Welcome to Family Physiotherapy's patient resource about Arthritis of the thumb injuries.
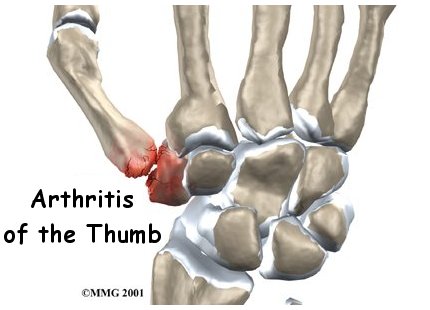
When you stop to think about how much you use your thumbs, it's easy to see why the joint where the thumb attaches to the hand can suffer from wear and tear. This joint is designed to give the thumb its rather large range of motion, but the tradeoff is that the joint suffers a lot of stress over the years. This can lead to painful osteoarthritis of this joint that may require surgical treatment as the arthritis progresses.
This guide will help you understand:
- how arthritis of the thumb develops
- how it is diagnosed
- what can be done for the condition
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Hand Pain|limit:15|heading:Hear from some of our patients who we treated for *Hand Pain*#
Anatomy
Where is the CMC joint, and what does it do?
The CMC joint (an abbreviation for carpometacarpal joint) of the thumb is where the metacarpal bone of the thumb attaches to the trapezium bone of the wrist. This joint is sometimes referred to as the basal joint of the thumb. The CMC is the joint that allows you to move your thumb into your palm, a motion called opposition.
Carpometacarpal Joint
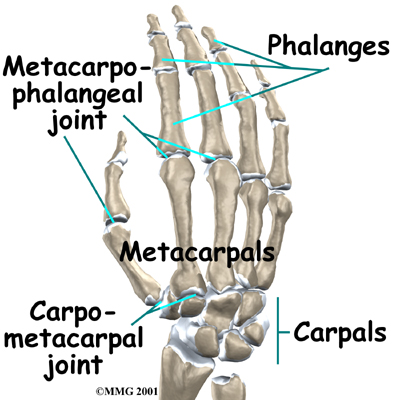
Trapezium Bone
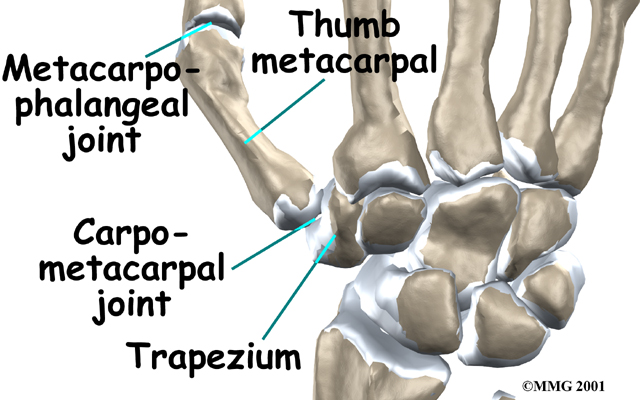
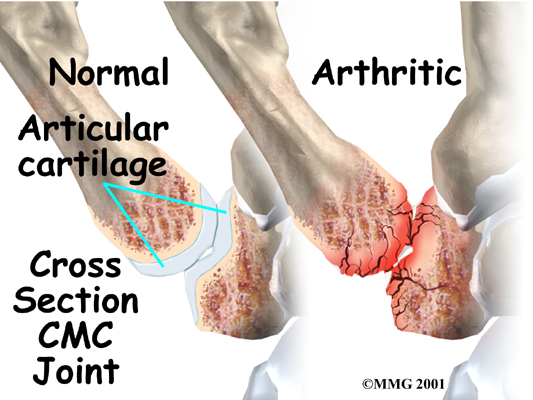
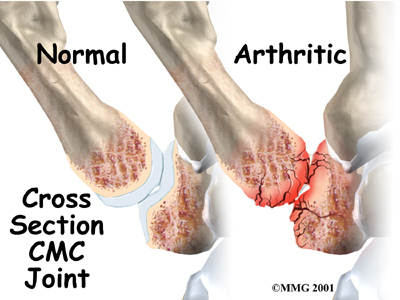
Several ligaments hold the CMC joint together. These ligaments can be injured, such as when you sprain your thumb. The joint surfaces are covered with a material called articular cartilage. This material is the slick, spongy covering that allows one side of a joint to slide against the other joint surface easily.
Articular Cartilage
Related Document: Family Physiotherapy's Guide to Hand Anatomy
Causes
What causes arthritis of the thumb?
Arthritis is a condition in which a joint becomes inflamed (red, swollen, hot, and painful). Degenerative arthritis is a condition in which a joint wears out, usually slowly over a period of many years. Doctors sometimes also describe this same condition as degenerative arthrosis. It is also called osteoarthritis.
Degenerative Arthritis
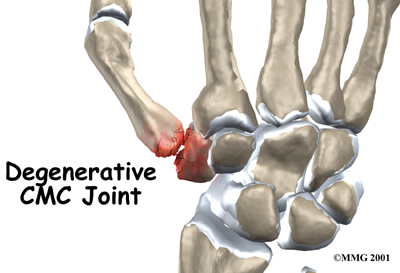
Injury to a joint, such as a bad sprain or fracture, can cause damage to the articular cartilage. An injury to the CMC joint of the thumb, even if it does not injure the articular cartilage directly, can alter how the joint works. After a fracture of the thumb metacarpal, the bone fragments may heal in slightly different positions. The joints may then line up differently. This is also true when the ligaments around the CMC joint are damaged by a sprain. When an injury results in a change in the way the joint moves, the injury may increase the forces on the articular cartilage surfaces. This is similar to any mechanical device or machinery. If the mechanism is out of balance, it tends to wear out faster.
Over many years this imbalance in the joint mechanics can lead to damage on the articular surface. Since articular cartilage cannot heal itself very well, the damage adds up. Eventually, the joint is no longer able to compensate for the increasing damage, and it begins to hurt. Damage has occurred well before the pain begins.
Symptoms
What does arthritis of the thumb feel like?
Pain is the main problem with degenerative arthritis of any joint. This pain occurs at first only related to activity. Usually, once the activity gets underway there is not much pain, but after resting for several minutes the pain and stiffness increase. Later, when the condition worsens, pain may be present even at rest. The most noticeable problem with CMC joint arthritis is that it becomes difficult to grip anything. It causes a sharp pain at the base of the thumb in the thick part of the heel of the hand.
Base of Thumb

When the articular cartilage starts to wear off the joint surface, the joint may make a squeaking sound when moved. Doctors refer to this sound as crepitus. The joint often becomes stiff and begins to lose motion. Moving the thumb away from the palm may become difficult. This is referred to as a contracture.
Osteoarthritis may cause the CMC joint of the thumb to loosen and to bend back too far (hyperextension). If the middle thumb joint (MCP joint) becomes flexed and the furthest thumb joint also becomes hyperextended, the deformity is named a thumb swan neck deformity. A similar finger deformity sometimes occurs in people with finger arthritis.
Thumb Swan Neck Deformity
Related Document: Family Physiotherapy's Guide to Swan Neck Deformity of the Finger
Diagnosis
When you visit Family Physiotherapy, our diagnosis of CMC joint arthritis of the thumb begins with our physiotherapist taking a detailed history of the problem. Specifics about any injuries that may have occurred to the hand are important because they may suggest other reasons why the condition exists.
Following the history, our physiotherapist will examine your hand and possibly other joints in your body. We will need to see how the motion of the CMC joint has been affected.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the physiotherapists at Family Physiotherapy have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Our Treatment
What can be done for CMC joint arthritis?
The treatment of degenerative arthritis of the CMC joint of the thumb can be divided into the nonsurgical means to control the symptoms and the surgical procedures that are available to treat the condition. Surgery is usually not considered until the symptoms have become impossible to control without it.
Non-surgical Rehabilitation
Treatment usually begins when the CMC joint first becomes painful. This may only occur with heavy use and may simply require mild anti-inflammatory medications, such as aspirin or ibuprofen. Ensure that you consult with your doctor or pharmacist regarding the use of pain relief or anti-inflammatory medication. Reducing the activity, or changing from occupations that require heavy repetitive gripping with the hand, may be necessary to help control the symptoms.
If you don't need surgery, your physiotherapist at Family Physiotherapy will first work with you to obtain or create a special thumb brace or splint when needed. These devices are designed to help reduce pain, prevent deformity, or keep a thumb deformity from getting worse. A thumb stabilizer is a type of thumb splint that is often custom-made of heat-moldable plastic. It is designed to fit the forearm, wrist, and thumb. Our patients with CMC joint arthritis usually only wear the splint at night and when the joint is flared up. It should also be worn to protect the thumb during heavy or repeated hand and thumb activities.
Our primary therapeutic goal is to help you learn how to control symptoms and maximize the health of your thumb. Our physiotherapist will teach you ways to calm pain and symptoms, which might include the use of rest, heat, or topical rubs.
We will begin instructing you in range-of-motion and stretching exercises to improve your thumb motion. Our program then advances to include strength exercises for the thumb and fingers. We use dexterity and fine motor exercises to get your hand and thumb moving smoothly. Your physiotherapist will also go over tips on how you can get your tasks done with less strain on the joint.
Although the time required for recovery varies among patients, as a guideline, you may expect to progress to a home program within four to six weeks.
Post-surgical Rehabilitation
After surgery, your hand will be bandaged with a well-padded dressing and a thumb splint for support. When you begin your physiotherapy program, the first few treatments are used to help control the pain and swelling after surgery.
Our physiotherapist will have you begin doing exercises to help strengthen and stabilize the muscles around the thumb joint. We’ll use other exercises to improve the fine motor control and dexterity of your hand. Our physiotherapist will also provide tips on ways to do your activities while avoiding extra strain on the thumb joint.
When your recovery is well under way, regular visits to Family Physiotherapy will end. Although we will continue to be a resource, you will eventually be in charge of doing your exercises as part of an ongoing home program.
Family Physiotherapy provides services for physiotherapy in Edmonton.
Physician Review
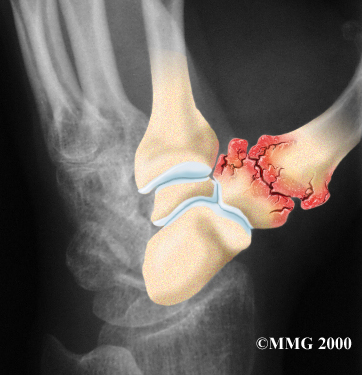
Your doctor may take X-rays to see how much the joint is damaged.
X-Rays

This test usually determines how bad the degenerative arthritis has become. How much articular cartilage remains in the joint can be estimated with the X-rays.
An injection of cortisone into the joint can give temporary relief. Cortisone is a very powerful anti-inflammatory medication. When injected into the joint itself, it can help relieve the pain. Pain relief is temporary and usually only lasts several weeks to months. There is a small risk of infection with any injection into the joint, and cortisone injections are no exception.
Cortisone Injection

Surgery
The surgical treatment for arthritis of the CMC joint includes several options. At one time, joint replacement with an artificial joint made with silicon was very popular. Problems with silicon implants in other parts of the body have led many surgeons to return to more traditional operations such as fusion and excision arthroplasty instead. Newer artificial joints are being developed, and in the future we may see more surgeons using them.
CMC Joint Fusion
A fusion, or arthrodesis, of any joint is designed to eliminate pain by allowing the bones that make up the joint to grow together, or fuse, into one solid bone. Fusions are used in many joints and were very common before the invention of artificial joints for the replacement of arthritic joints. Even today, joint fusions are still commonly used in many different joints for treating the pain of arthritis.
A fusion of the CMC joint of the thumb is done quite often in younger people who need a strong grip or pinch more than they need the fine motion of the thumb. People who use their hands for heavy work will probably prefer a fusion over an arthroplasty (described below).
Artificial Joint Replacement (Arthroplasty)
Artificial joints are available for the CMC joint. These plastic or metal prostheses are used by some hand surgeons to replace the joint. The prosthesis acts as a spacer to fill the gap created when the arthritic surfaces of the two bones that make up the CMC joint are removed.
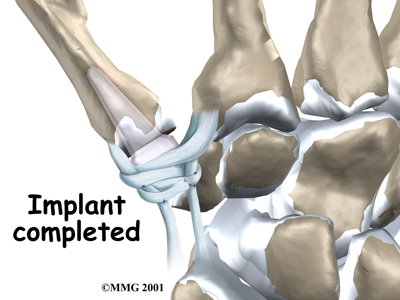
Excision Arthroplasty
The traditional operation for treating CMC joint arthritis is excision arthroplasty. This method has been used for many years and has withstood the test of time. The purpose of excision arthroplasty is to remove the arthritic joint surfaces of the CMC joint and replace them with a cushion of material that will keep the bones separated. Most surgeons use a piece of tendon that has been rolled up and placed into the space created by removing the bone surfaces. During the healing phase after surgery, this tendon turns into tough scar tissue that forms a flexible connection between the bones, similar to a joint.
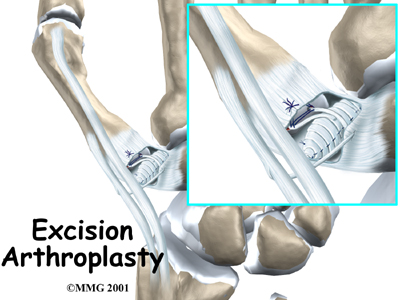
This operation is also combined with a reconstruction of the joint where tendons in the area are used to create a ligament sling between the metacarpal bone of the thumb and the carpal bone of the index finger. This helps hold the thumb in place and keeps the space between the bones from collapsing.
Portions of this document copyright MMG, LLC.
