Lumbar Degenerative Disc Disease
Introduction
Physiotherapy in Edmonton for Lower Back

Welcome to Family Physiotherapy's patient resource about Lumbar Degenerative Disc Disease.
The intervertebral discs in the lower spine are commonly blamed for low back pain. Yet low back pain has many possible causes, and doctors aren't always certain why symptoms occur.
During an office visit for low back pain, your doctor may describe how changes in the discs can lead to back pain. When talking about these changes, your doctor may use the terms degeneration or degenerative disc disease. Although the parts of the spine do change with time and in some sense degenerate, this does not mean the spine is deteriorating and that you are headed for future pain and problems. These terms are simply a starting point for describing what occurs in the spine over time, and how the changes may explain the symptoms people feel.
This guide will help you understand:
- how degenerative disc disease develops
- how doctors diagnose the condition
- what treatment options are available
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Back Pain|limit:15|heading:Hear from some of our patients who we treated for *Back Pain*#
Anatomy
What parts of the spine are involved?
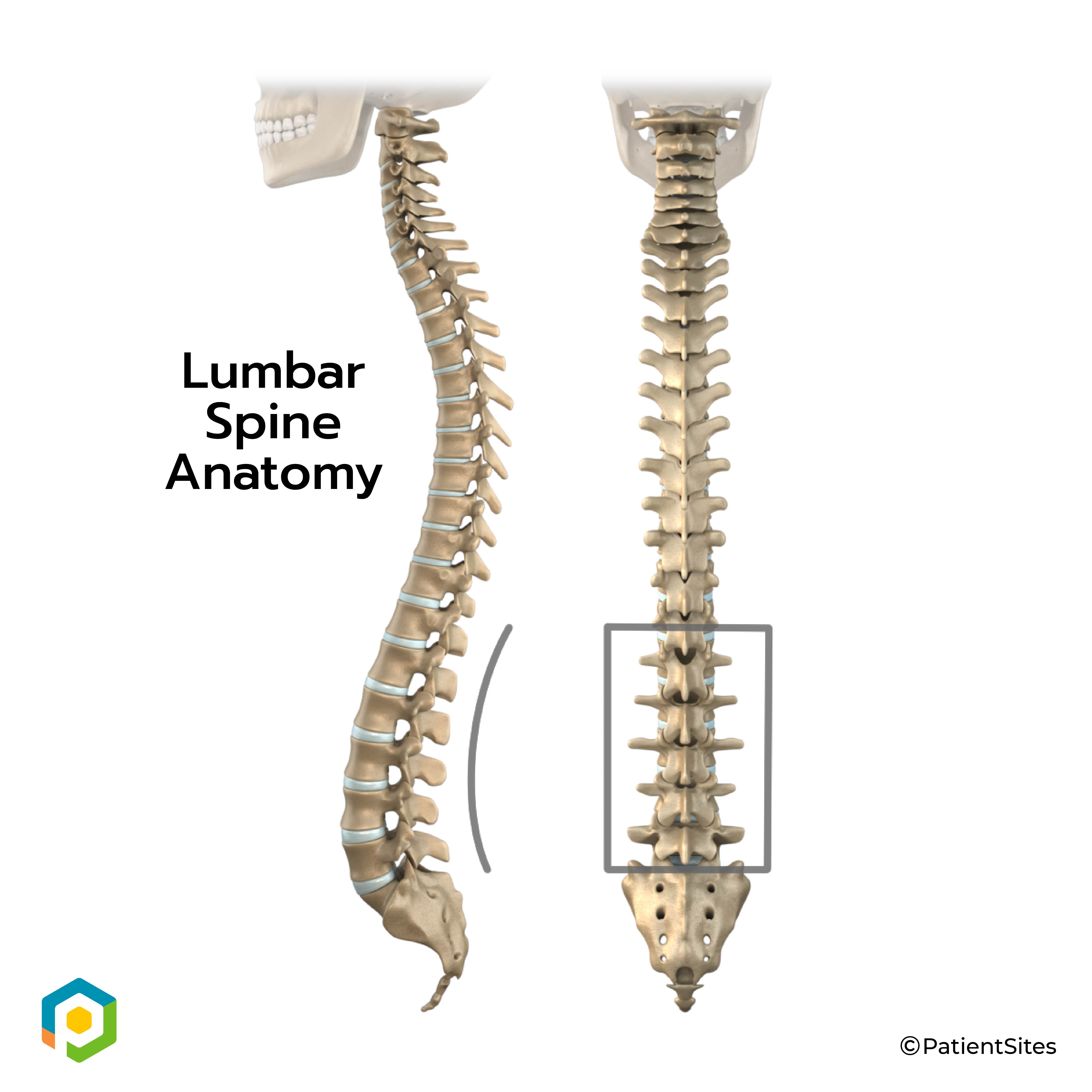
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to form the spinal column. The spinal column gives the body its form. It is the body's main upright support. The section of the spine in the lower back is known as the lumbar spine.
Lumbar Spine
An intervertebral disc sits between each pair of vertebrae. The intervertebral disc is made of connective tissue. Connective tissue is the material that holds the living cells of the body together. Most connective tissue is made of fibers of a material called collagen. These fibers help the disc withstand tension and pressure.
Intervertebral Disc
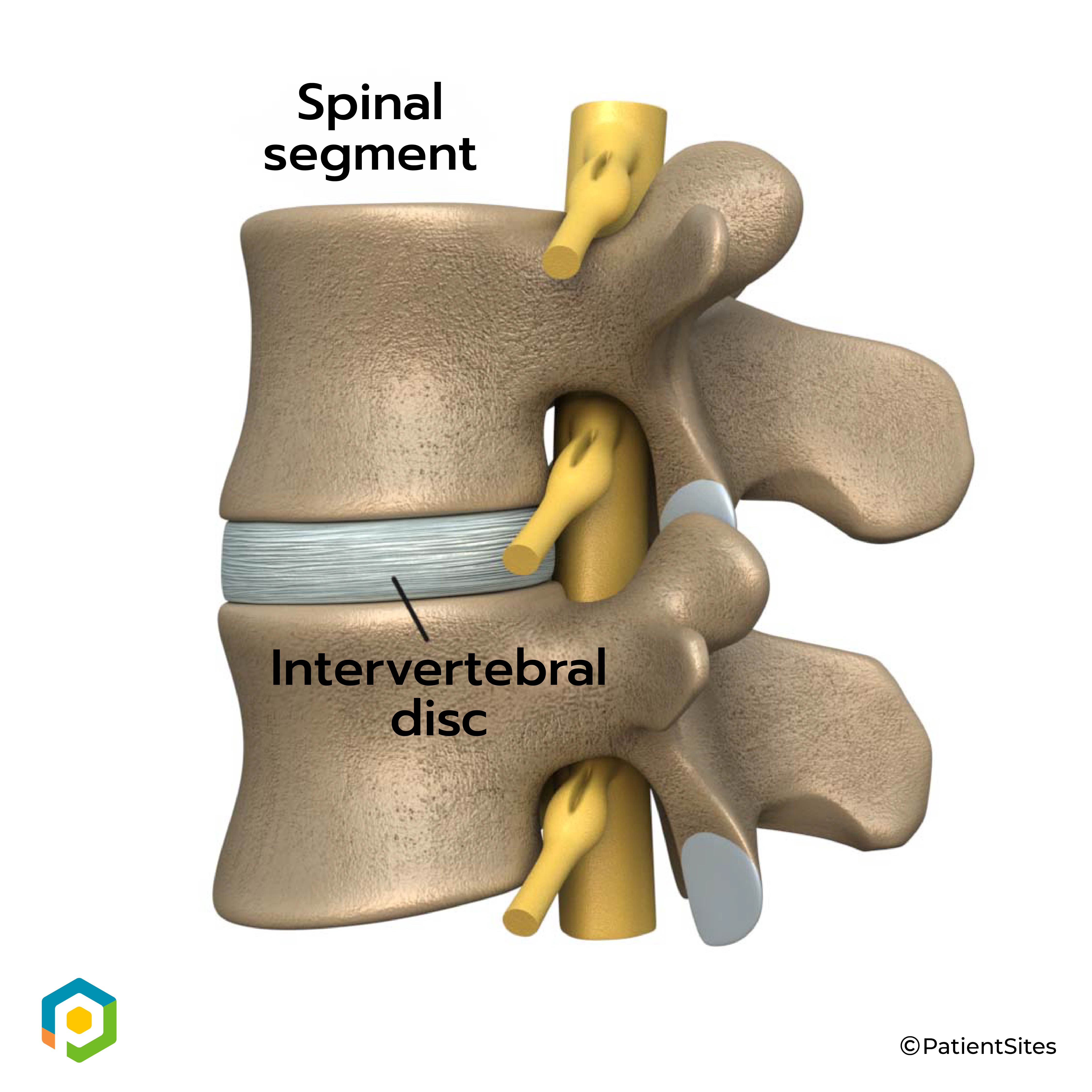
The disc normally works like a shock absorber. It protects the spine against the daily pull of gravity. It also protects the spine during strenuous activities that put strong force on the spine, such as jumping, running, and lifting.
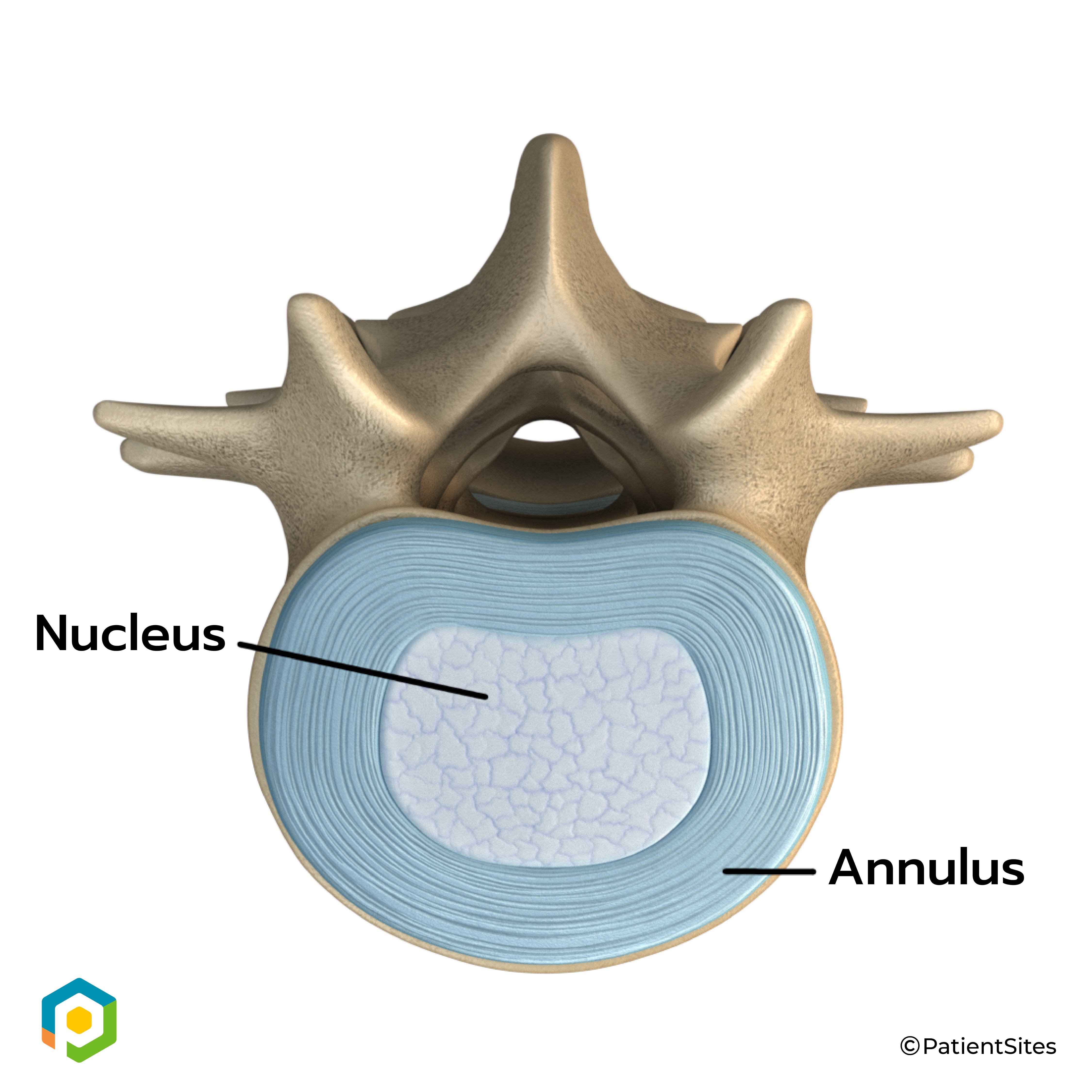
An intervertebral disc is made of two parts. The center, called the nucleus, is spongy. It provides most of the disc's ability to absorb shock. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are connective tissues that attach bones to other bones.
Two Parts of Intervertebral Disc
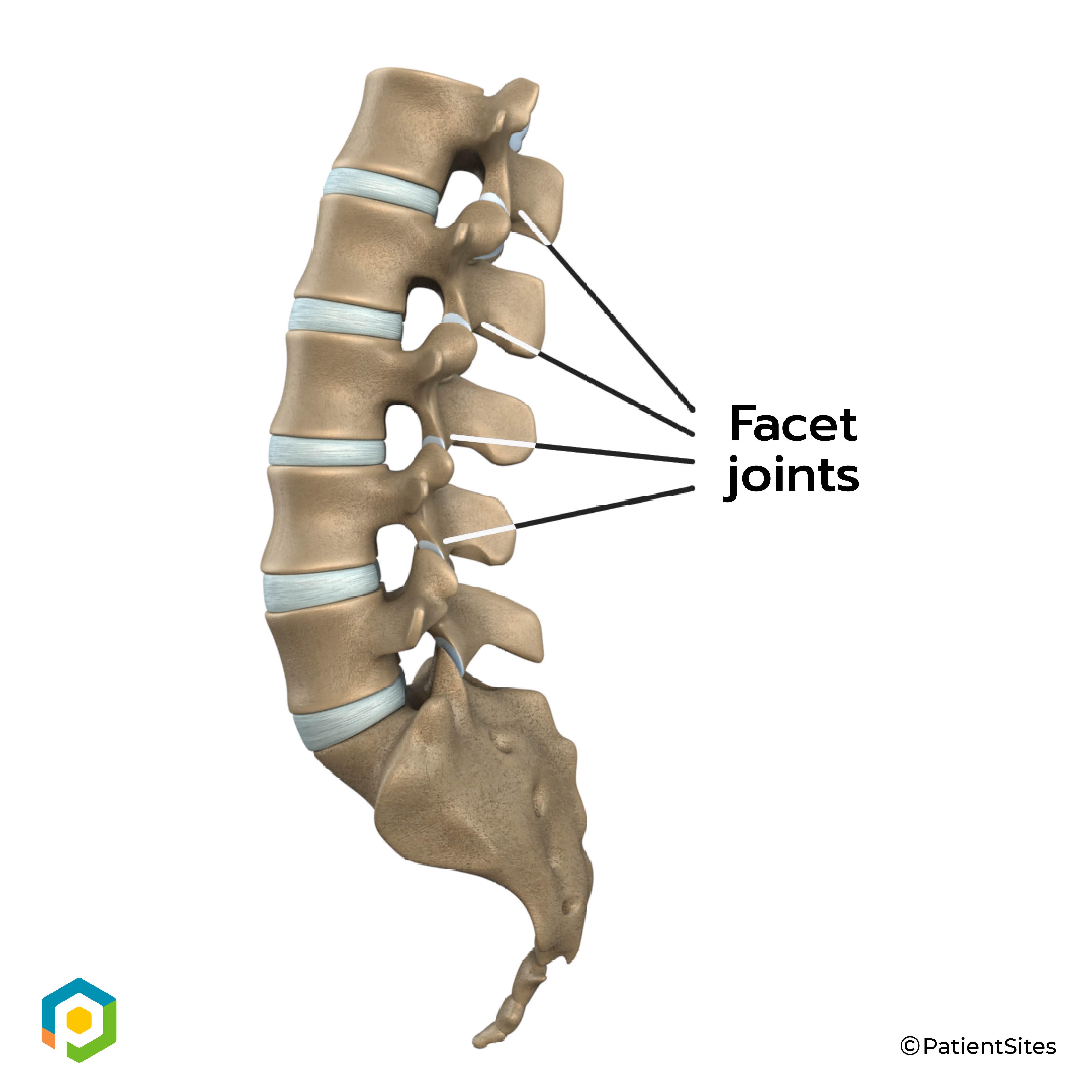
Between the vertebrae of each spinal segment are two facet joints. The facet joints are located on the back of the spinal column. There are two facet joints between each pair of vertebrae, one on each side of the spine. A facet joint is made of small, bony knobs that line up along the back of the spine. Where these knobs meet, they form a joint that connects the two vertebrae. The alignment of the facet joints of the lumbar spine allows freedom of movement as you bend forward and back.
Facet Joints
Related Document: Family Physiotherapy's Guide to Lumbar Spine Anatomy
Causes
Why do I have this problem?
Our intervertebral discs change with age, much like our hair turns gray. Conditions such as a major back injury or fracture can affect how the spine works, making the changes happen even faster. Daily wear and tear and certain types of vibration can also speed up degeneration in the spine. In addition, strong evidence suggests that smoking speeds up degeneration of the spine. Scientists have also found links among family members, showing that genetics play a role in how fast these changes occur.
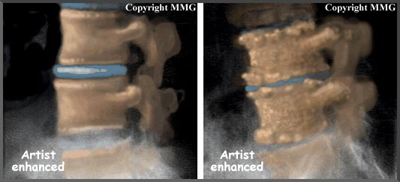
Disc degeneration follows a predictable pattern. First, the nucleus in the center of the disc begins to lose its ability to absorb water. The disc becomes dehydrated. Then the nucleus becomes thick and fibrous, so that it looks much the same as the annulus. As a result, the nucleus isn't able to absorb shock as well. Routine stress and strain begin to take a toll on the structures of the spine. Tears form around the annulus. The disc weakens. It starts to collapse, and the bones of the spine compress.
Related Document: Family Physiotherapy's Guide to Low Back Pain
This degeneration does not always mean the disc becomes a source of pain. In fact, X-rays and MRI scans show that people with severe disc degeneration don't always feel pain.
Pain caused by degenerative disc disease is mainly mechanical pain, meaning it comes from the parts of the spine that move during activity: the discs, ligaments, and facet joints. Movement within the weakened structures of the spine causes them to become irritated and painful.
Symptoms
 What does the condition feel like?
What does the condition feel like?
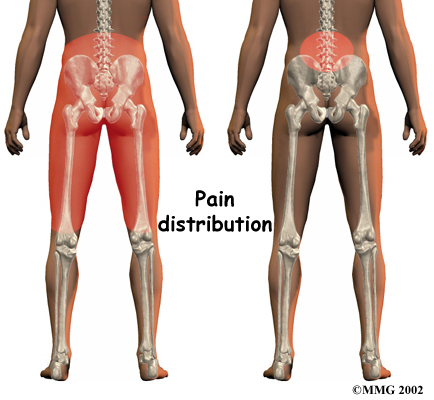
Pain in the center of the low back is often the first symptom patients feel. It usually starts to affect patients in their twenties and thirties. Pain tends to worsen after heavy physical activity or staying in one posture for a long time. The back may also begin to feel stiff. Resting the back eases pain. At first, symptoms only last a few days.
This type of back pain often comes and goes over the years. Doctors call this recurring back pain. Each time it strikes, the pain may seem worse than the time before. Eventually the pain may spread into the buttocks or thighs, and it may take longer for the pain to subside.
Diagnosis
How do health care providers diagnose the problem?
Diagnosis begins with a complete history and physical exam. When you visit Family Physiotherapy, we will ask questions about your symptoms and how your problem is affecting your daily activities. Our physiotherapist will also want to know what positions or activities make your symptoms worse or better.
Our physiotherapist then does a physical examination by checking your posture and the amount of movement in your low back. We check to see which back movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are also tested.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the physiotherapists at Family Physiotherapy have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Family Physiotherapy provides services for physiotherapy in Edmonton.
Our Treatment
Non-surgical Rehabilitation
Whenever possible, nonsurgical treatment of lumbar degenerative disc disease is preferred. The first goal of nonsurgical treatment is to ease pain and other symptoms so the patient can resume normal activities as soon as possible.
We rarely prescribe bed rest for patients with degenerative disc problems. Instead, patients are encouraged to do their normal activities using pain as a gauge for how much is too much. If symptoms are severe, a maximum of typically two days of bed rest may be prescribed.
After evaluating your condition, your physiotherapist at Family Physiotherapy can assign positions and exercises to ease symptoms. Our physiotherapist can design a personalized exercise program to improve flexibility of tight muscles, to strengthen the back and abdominal muscles, and to help you move safely and with less pain. Although recovery time varies among patients, as a guideline you may expect to work with our physiotherapist a few times each week for four to six weeks. In some cases, patients may need a few additional weeks of care.
Our first goal of treatment is to control symptoms. Your physiotherapist will work with you to find positions and movements that ease pain. We may use heat, cold, ultrasound, and electrical stimulation to calm pain and muscle spasm.
Our physiotherapist may perform hands-on treatments such as massage and specialized forms of soft-tissue mobilization. These can help a patient begin moving with less pain and greater ease. Traction is also a common treatment for degenerative disc problems. Traction gently stretches the low back joints and muscles. Our physiotherapist will instruct you on stretches that will help you move easier and with less pain.
As you recover, we will gradually advance you in a series of strengthening exercises for the abdominal and low back muscles. Working these core muscles helps patients move more easily and lessens the chances of future pain and problems.
A primary purpose of physiotherapy is to help you learn how to take care of your symptoms and prevent future problems. We’ll give you a home program of exercises to continue improve flexibility, posture, endurance, and low back and abdominal strength. Our physiotherapist will also discuss strategies you can use if your symptoms flare up.
Post-surgical Rehabilitation
Rehabilitation after surgery is more complex. Some patients leave the hospital shortly after surgery. However, some surgeries require patients to stay in the hospital for a few days.
During recovery from surgery, patients should follow their surgeon's instructions about wearing a back brace or support belt. You should be cautious about overdoing activities in the first few weeks after surgery.
Many surgical patients need physiotherapy outside of the hospital. Patients who've had lumbar fusion surgery normally need to wait up to three months before beginning a rehabilitation program. Our treatment sessions help patients build strength and learn to move and do routine activities without putting extra strain on their backs.
Although the length of Family Physiotherapy rehabilitation programs vary based on an individual patient’s rate of recovery, as a guideline you can expect to attend physiotherapy sessions for eight to 12 weeks and should expect full recovery to take up to six months.
As your physiotherapy sessions come to an end, our physiotherapist will help you get back to the activities you enjoy. You may need guidance on which activities are safe or how to change the way you go about your activities. Ideally, patients are able to resume normal activities.
When recovery is well under way, regular visits to Family Physiotherapy will end. Although we will continue to be a resource, you will be are in charge of doing your exercises as part of an ongoing home program.
Family Physiotherapy provides services for physiotherapy in Edmonton.
Physician Review
Doctors rely on the history and physical exam to determine which treatments will help the most. X-rays are rarely ordered on the first doctor visit for this problem. This is because over 30 percent of low back X-rays show abnormalities from degeneration, even in people who aren't having symptoms.
However, if symptoms are severe and aren't going away, the doctor may order an X-ray. The test can show if one or more discs has started to collapse. It can also show if there are bone spurs in the vertebrae and facet joints. Bone spurs are small points of bone that form with degeneration.
When more information is needed, your doctor may order a magnetic resonance imaging (MRI) scan. The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. It is helpful for showing if the tissues in the disc are able to absorb water and whether there are cracks inside the disc. It can also show if there are problems in other soft tissues, such as the spinal nerves.
Discography can help with the diagnosis. This is a specialized X-ray test in which dye is injected into one or more discs. The dye is seen on X-ray and can give some information about the health of the disc or discs. This test may be done when the surgeon is considering surgery, since it can help determine which disc is causing the symptoms.
 Back braces are sometimes prescribed. Keeping the moving parts of the low back still can help calm mechanical pain. When a doctor issues a brace, he or she normally asks that the patient only wear it for two to four days. This lessens the chance that the trunk muscles will shrink (atrophy) from relying on the belt.
Back braces are sometimes prescribed. Keeping the moving parts of the low back still can help calm mechanical pain. When a doctor issues a brace, he or she normally asks that the patient only wear it for two to four days. This lessens the chance that the trunk muscles will shrink (atrophy) from relying on the belt.
Patients may also be prescribed medication by their physician to help them gain control of their symptoms so they can resume normal activity swiftly.
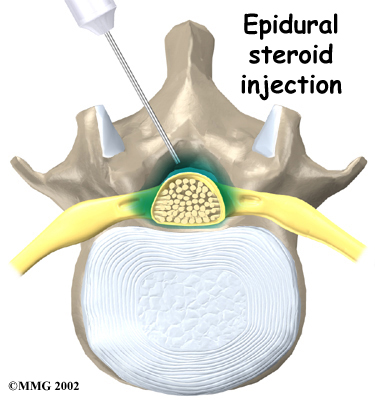
If symptoms continue to limit a person's ability to function normally, the doctor may suggest an epidural steriod injection (ESI). Steroids are powerful anti-inflammatories, meaning they help reduce pain and swelling. In an ESI, medication is injected into the space around the lumbar nerve roots. This area is called the epidural space. Some doctors inject only a steroid. Most doctors, however, combine a steroid with a long-lasting numbing medication. Generally, an ESI is given only when other treatments aren't working. But ESIs are not always successful in relieving pain. If they do work, they often only provide temporary relief.
Surgery
 People with degenerative disc problems tend to gradually improve over time. Most do not need surgery. In fact, only one to three percent of patients with degenerative disc problems typically require surgery.
People with degenerative disc problems tend to gradually improve over time. Most do not need surgery. In fact, only one to three percent of patients with degenerative disc problems typically require surgery.
Doctors prefer to try nonsurgical treatment for a minimum of three months before considering surgery. If, after this period, nonsurgical treatment hasn't improved symptoms, the doctor may recommend surgery. The main types of surgery for degenerative disc problems include
- lumbar laminectomy
- discectomy
- fusion
Lumbar Laminectomy
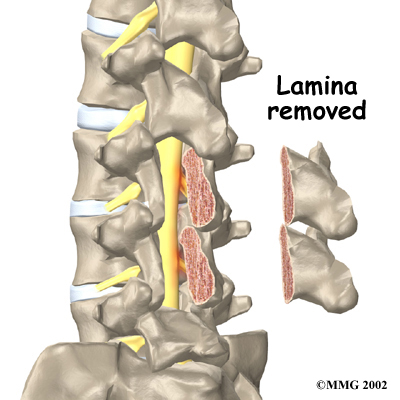
The lamina forms a roof-like structure over the back of the spinal column. When the nerves in the spinal canal are squeezed by a degenerated disc or by bone spurs pushing into the canal, a laminectomy removes most, or all of the lamina to release pressure on the spinal nerves.
Related Document: Family Physiotherapy's Guide to Lumbar Laminectomy
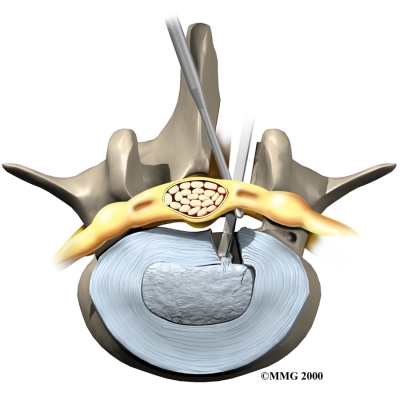 Discectomy
Discectomy
Surgery to take out part or all of a problem disc in the low back is called discectomy. Discectomy is done when the degenerated disc has ruptured (herniated) into the spinal canal, putting pressure on the spinal nerves. Surgeons commonly perform this operation through an incision in the low back. Before the disc material can be removed, the surgeon must first remove part of the lamina. Generally, only a small piece of the lamina is chipped away to expose the problem disc. This is called laminotomy. It usually creates enough room for the surgeon to remove the disc. If more room is needed, the surgeon may need to take out a larger section of the lamina by doing a laminectomy (described above).
Many surgeons now do minimally invasive surgeries that require only small incisions in the low back. These procedures are used to remove damaged portions of the problem disc. Advocates believe that this type of surgery is easier to perform. They also believe it prevents scarring around the nerves and joints and helps patients recover more quickly. Minimally invasive surgeries include percutaneous lumbar discectomy, laser discectomy, and microdiscectomy.
Related Document: Family Physiotherapy's Guide to Lumbar Discectomy
Fusion
Fusion surgery joins two or more bones into one solid bone. This prevents the bones and joints from moving. The procedure is sometimes done with a discectomy. Mechanical pain is eased because the fusion holds the moving parts steady, so they can't cause irritation and inflammation.
The main types of fusion for degenerative disc problems include
- anterior lumbar interbody fusion
- posterior lumbar fusion
- combined fusion
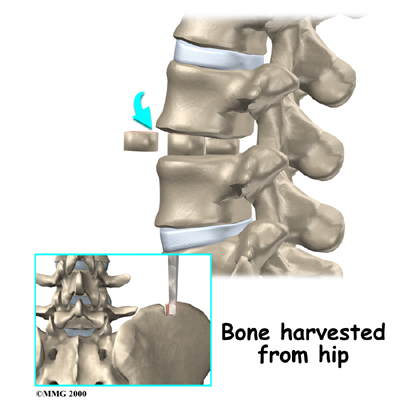
Anterior Lumbar Interbody Fusion
Anterior lumbar interbody fusion surgery is done through the abdomen, allowing the surgeon to work on the anterior (front) of the lumbar spine. Removing the disc (discectomy) leaves a space between the pair of vertebrae. This interbody space is filled with a bone graft. One method is to take a graft from the pelvic bone and tamp it into place. Another method involves inserting two hollow titanium screws packed with bone, called fusion cages, into the place where the disc was taken out. The bone graft inside the cages fuses with the adjacent vertebrae, forming one solid bone.
Bone Graft
Related Document: Family Physiotherapy's Guide to Anterior Lumbar Fusion with Cages
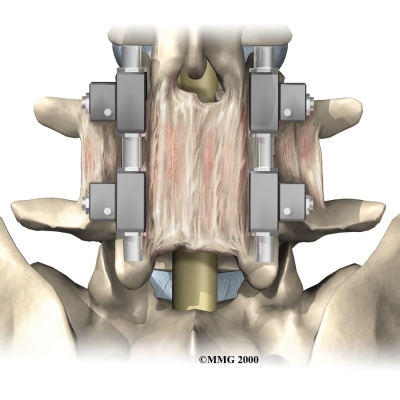
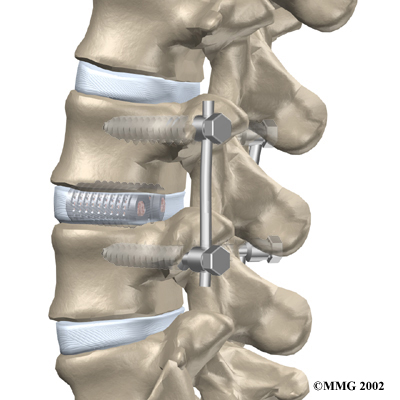
Posterior Lumbar Fusion
A posterior lumbar fusion is done though an incision in the back. In this procedure, the surgeon lays small grafts of bone over the problem vertebrae. Most surgeons will also apply metal plates and screws to hold the vertebrae in place while they heal. This protects the graft so it can heal better and faster.
Metal Plates and Screws
Related Document: Family Physiotherapy's Guide to Posterior Lumbar Fusion
Combined Fusion
A combined fusion involves fusing the anterior (front) and posterior (back) surfaces of the problem vertebrae. By locking the vertebrae from the front and back, some surgeons believe the graft stays solid and is prevented from collapsing. Results do show improved fusion of the graft, though patients seem to fare equally well with other methods of fusion.
Portions of this document copyright MMG, LLC.
