Anterior Lumbar Fusion with Cages
Introduction
Physiotherapy in Edmonton for Lower Back
Welcome to Family Physiotherapy's patient resource about Anterior Lumbar Fusion with Cages.
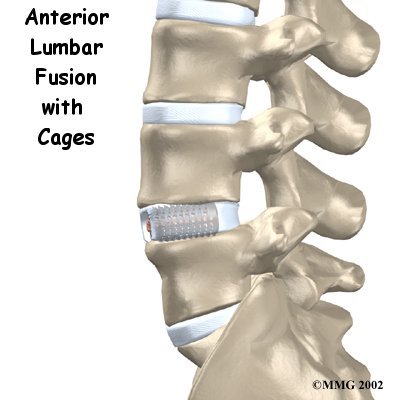
Anterior lumbar fusion is an operation done on the front (the anterior region) of the lower spine. Fusion surgery helps two or more bones grow together into one solid bone. Fusion cages are new devices, essentially hollow screws filled with bone graft, that help the bones of the spine heal together firmly. Surgeons use this procedure when patients have symptoms from disc degeneration, disc herniation, or spinal instability.
Anterior Region
This article will help you understand:
- why the procedure becomes necessary
- what surgeons hope to achieve
- what to expect during your recovery
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Back Pain|limit:15|heading:Hear from some of our patients who we treated for *Back Pain*#
Anatomy
What parts of the spine are involved?
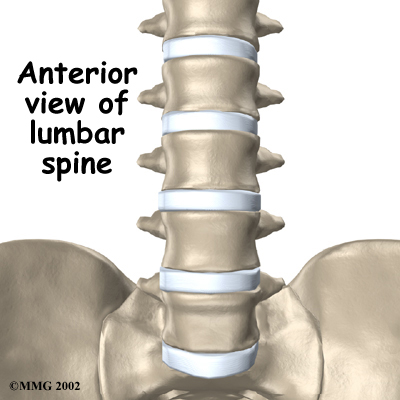
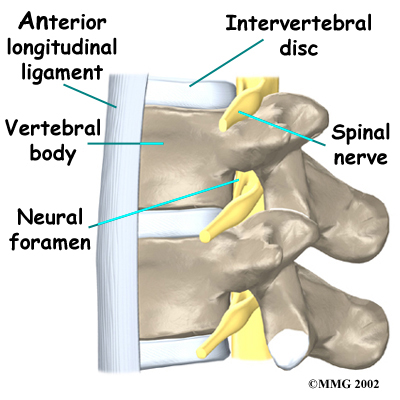
Since the surgeon needs to reach the front of the spine, this operation is done through the abdomen. The main structures involved in this procedure are the vertebral bodies and the intervertebral discs. The vertebral bodies are the large blocks of bone that make up the front section of each vertebra. The intervertebral discs are the cushions between each pair of vertebrae. The fusion cages help separate the vertebral bodies, taking pressure off the spinal nerves where they travel from the spinal canal through openings called the neural foramen.
Main Stuctures
 Vertebra
Vertebra
Related Document: Family Physiotherapy's Guide to Lumbar Spine Anatomy
Rationale
What do surgeons hope to achieve?
In most cases, this procedure is used to stop symptoms from lumbar disc disease. The intervertebral discs in the spine degenerate as a natural part of aging. Daily wear and tear and certain types of vibration can also speed up degeneration in the spine. In addition, strong evidence suggests that smoking speeds up degeneration of the spine. Scientists have also found links among family members, showing that genetics plays a role in how fast these changes occur. When degeneration occurs, a problem disc begins to collapse, and the space decreases between the vertebrae.
Related Document: Family Physiotherapy's Guide to Lumbar Degenerative Disc Disease
When this happens, the opening around the spinal nerves (the neural foramen) narrows and may begin to put pressure on the nerves. The long ligaments in the spine slacken. They may even buckle and put pressure on the spinal nerves. The outer rings of the disc, the annulus, weaken and develop small cracks. The nucleus in the center of the disc presses on the weakened annulus and may actually squeeze through the annulus and press on ligaments or nerves. Fragments of the disc that press against the outer annulus and spinal nerves can be a source of pain, numbness, and weakness. Pressure on the spinal nerves can also produce problems with the bowels and bladder, requiring emergency surgery.
View animation of degeneration
A fusion operation can reduce or eliminate the pain caused by a problem disc. If the fusion is successful, the vertebrae that are fused together no longer move against one another. Instead, they move together as one unit. This prevents the disc from causing pain.
Fusion cages are also designed to separate and hold the vertebrae apart. Enlarging the space between two vertebrae widens the opening of the neural foramina, taking pressure off the spinal nerves that pass through them. Also, the extra space pulls taut the ligaments inside the spinal canal so they don't buckle into the spinal canal.
View animation of regaining disc height
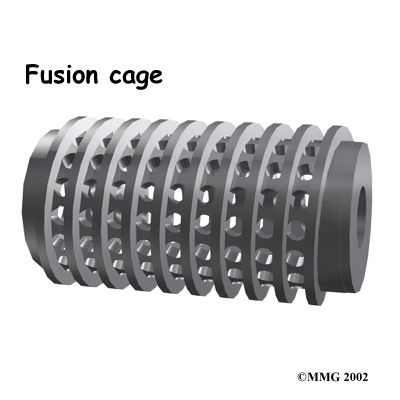
Fusion cages are most commonly made of metal, graphite, or bone. Many of these cages are shaped like cylinders. A few are rectangular in shape. They are usually threaded like a screw on the outside and hollow on the inside. The main purpose of the cage, regardless of the shape or material, is to hold the two vertebrae apart while the fusion becomes solid.
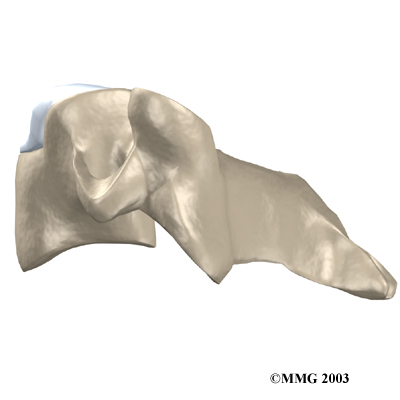
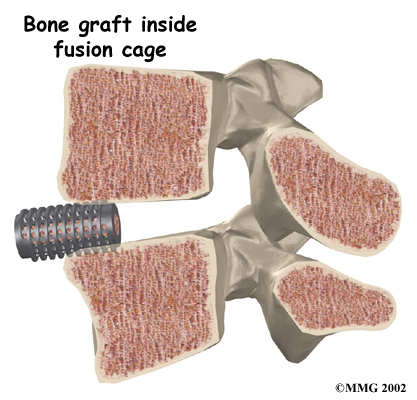
The surgeon packs the hollow center of the cage with bone. The graft is commonly taken from another part of the body, usually the top of the pelvis bone. Bone taken from another part of your own body is called an autograft. There is a risk of pain, infection, or weakness in the area where the graft is taken.
A new method to avoid this problem is with a bone graft substitute. By using gene therapy, scientists have produced bone graft substitutes called growth factors. These growth factors are natural proteins found in the human body. Genetic engineers have been able to clone proteins known as bone morphogenic proteins (BMPs). These proteins are then made available as powder, small particles, or chips. Hormones that circulate in the bloodstream act on the BMP molecules, causing them to build new bone tissue.
The growth factor that is approved for lumbar fusion with titanium cages is BMP-2. Substituting BMP-2 for an autograft eliminates the complications that go with harvesting autograft material from the patient's own body. This allows for shorter operation times, less loss of blood during surgery, and quicker recovery times for patients. New research shows that BMP-2 is at least as good as, and maybe even better than, autograft for anterior lumbar fusion with cages.
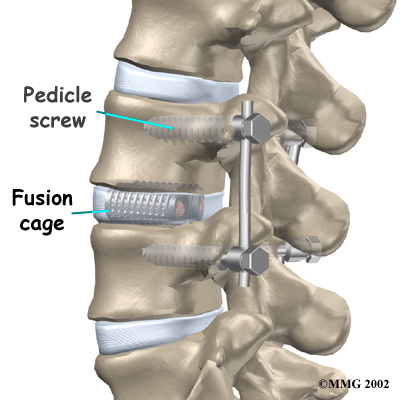
The surgeon packs the hollow center of the fusion cages with bone graft, either in the form of an autograft or bone graft substitute. Two cages are placed side by side within the disc. The cages spread the vertebrae apart, and the threads bind the vertebrae to keep them from moving. After implanting the cages, most surgeons attach metal hardware on the vertebrae to rigidly lock them in place. This helps the bone graft heal, fusing the vertebrae together.
Once the bones fuse, they are prevented from moving against one another. This helps relieve the mechanical pain, which occurs in the moving parts of the back. Fusion also prevents additional wear and tear on the structures inside the section that was fused. By fusing the bones together, surgeons hope to reduce future problems at the spinal segment.
Preparations
How will I prepare for surgery?
The decision to proceed with surgery must be made jointly by you and your surgeon. You should understand as much about the procedure as possible. If you have concerns or questions, talk to your surgeon.
Once you decide on surgery, your surgeon may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn't eat or drink anything after midnight the night before.
Surgical Procedure
 What happens during the operation?
What happens during the operation?
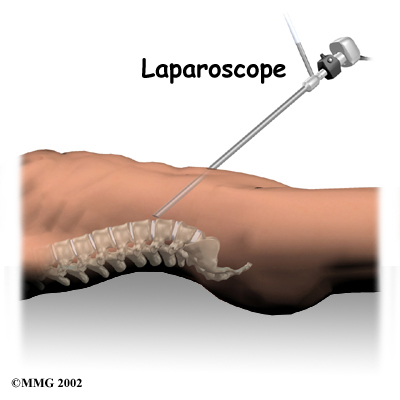
Traditionally, this operation requires a sizeable abdominal incision. Recently, however, surgeons have begun using a laparoscope in this operation. A laparoscope is a small television camera that lets the surgeon see inside the abdominal cavity to perform the operation. Several much smaller abdominal incisions are needed in the laparoscopic method. The smaller incisions allow patients to begin moving sooner and healing faster. However, performing anterior lumbar fusion with a laparoscope is difficult. It isn't the right choice for all fusion surgeries.
Patients are positioned on their backs with a pad placed under the low back. They are given general anesthesia to put them to sleep. As they sleep, their breathing may be assisted with a ventilator. A ventilator is a device that controls and monitors the flow of air to the lungs.
In the traditional method, an incision is made through one side of the abdomen. Organs and blood vessels are gently moved aside to expose the front of the lumbar spine.
The problem disc is located with a fluoroscope, a special X-ray that shows images on a TV screen. The surgeon drills two large holes horizontally through the front of the disc. The fusion cages are sized to fit into the newly drilled holes. Bone graft may be taken from the top of the pelvis. The other option is for the surgeon to use a bone graft substitute. The bone graft material is packed into the hollow cages. Then the surgeon screws the cages into the holes in the disc. The threads of the cages clinch the vertebrae above and below, holding them rigidly in place. The fluoroscope is used to check the position and fit of the cages.
Bone Graft - Screwing Cages into Disc Holes
As mentioned earlier, the surgeon may also fix the vertebrae in place using metal screws or plates. One option is screwing a strap of metal across the front of the spine. A second method involves additional surgery through the low back. This may be done on the same day or during a later surgery. Metal plates or screws applied through the back of the spine lock the two vertebrae and prevent them from moving. This protects the graft so it can heal better and faster.
Related Document: Family Physiotherapy's Guide to Posterior Lumbar Fusion
A drainage tube may be placed in the wound. The muscles and soft tissues are put back in place, and the skin is stitched together. The surgeon may place the patient in a rigid brace.
The threaded cages rigidly connect the vertebrae above and below. Small openings in the surface of the cages allow the bone graft inside to contact the surfaces of both vertebrae. As the new bone inside the cages heals to the nearby vertebrae, the two vertebrae become rigidly fused into one solid bone.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. Some of the most common complications following anterior lumbar fusion with cages include
- problems with anesthesia
- thrombophlebitis
- infection
- nerve damage
- blood vessel damage
- problems with the graft or hardware
- nonunion
- ongoing pain
This is not intended to be a complete list of the possible complications.
Problems with Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation. It occurs when the blood in the large veins of the leg forms blood clots. This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Most surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection following spine surgery is rare but can be a very serious complication. Some infections may show up early, even before you leave the hospital. Infections on the skin's surface usually go away with antibiotics. Deeper infections that spread into the bones and soft tissues of the spine are harder to treat. They may require additional surgery to treat the infected portion of the spine.
 Nerve Damage
Nerve Damage
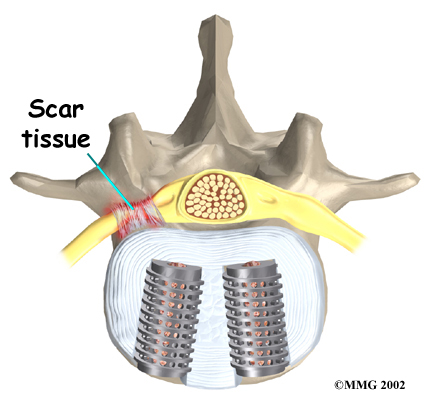
Any surgery that is done near the spinal canal can potentially cause injury to the spinal cord or spinal nerves. Injury can occur from bumping or cutting the nerve tissue with a surgical instrument, from swelling around the nerve, or from the formation of scar tissue. An injury to the spinal cord or spinal nerves can cause muscle weakness and a loss of sensation to the areas supplied by the nerve.
Blood Vessel Damage
The abdominal aorta (the largest artery in the body) and the large veins that accompany it run in front of the spine as they split to run to each leg. These vessels must be moved aside to perform the anterior cage procedure. Because of this, the vessels may be injured, causing bleeding. When the procedure is performed using the laparoscope, too much bleeding may require opening the abdomen with a larger incision to repair the injured vessels.
Problems with the Graft or Hardware
Fusion surgery with cages requires bone grafting. The graft is commonly taken from the top rim of the pelvis (autograft). As mentioned earlier, there is a risk of pain, infection, or weakness in the area where the graft is taken. These risks are avoided when a bone graft substitute, such as BMP-2, is used in place of an autograft.
After the cages are in place, the surgeon checks their position before completing the surgery. However, the cages may shift slightly soon after surgery to the point that they are no longer able to hold the spine stable. Abnormal or excessive loads on the spine, for example from heavy lifting or carrying or from the impact of jumping from a high surface, can cause the cages to collapse. This shifting or collapsing of the cages can cause injury to the nearby tissues. If this happens, a second surgery may be needed to replace the cages and to apply additional instrumentation to lock the spine firmly in place.
 Hardware can also cause problems. Screws or pins may loosen and irritate the nearby soft tissues. Also, the metal plates can sometimes break. If this happens, the surgeon may suggest another surgery either to take out the hardware or to add more hardware to solve the problem.
Hardware can also cause problems. Screws or pins may loosen and irritate the nearby soft tissues. Also, the metal plates can sometimes break. If this happens, the surgeon may suggest another surgery either to take out the hardware or to add more hardware to solve the problem.
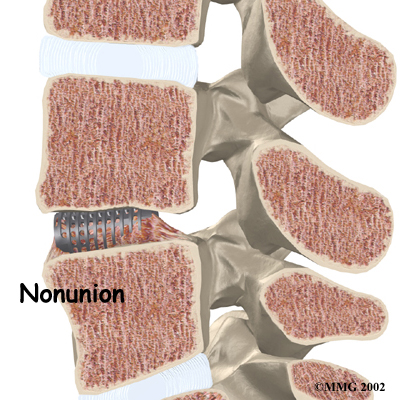
Nonunion
Sometimes the bones do not fuse as planned. This is called a nonunion, or pseudarthrosis. (The term pseudarthrosis means false joint.) When more than one level of the spine is fused at one time, there is a greater chance that nonunion will occur. Fusion of more than one level means two or more consecutive discs are removed and replaced with bone graft. If the joint motion from a nonunion causes pain, you may need a second operation.
In the second procedure, the surgeon may have to replace the cages. Metal plates and screws may also be added to rigidly secure the bones so they will fuse.
Ongoing Pain
Anterior lumbar fusion with cages is a complex surgery. Not all patients get complete pain relief with this procedure. As with any surgery, you should expect some pain afterward. If the pain continues or becomes unbearable, talk to your surgeon about treatments that can help control your pain.
After Surgery
What happens after surgery?
Patients are sometimes placed in a rigid body brace after surgery. This brace may not be needed if the surgeon attached metal hardware to the spine during the surgery.
Patients usually stay in the hospital after surgery for up to one week. During this time, a physiotherapist helps patients learn safe ways to move, dress, and do activities without putting extra strain on the back. Patients may be instructed to use a walker for the first day or two. Before going home, patients are shown how to control pain and avoid problems.
Patients are able to return home when their medical condition is stable. However, they are usually required to keep their activities to a minimum in order to give the graft time to heal. Patients are cautioned against bending forward, lifting, twisting, driving, and prolonged sitting for up to six weeks. Activities and exercises that cause the spine to bend back place hazardous stress on the cages and should be avoided for at least six months. Outpatient physiotherapy usually begins a minimum of six weeks after the date of surgery.
Our Rehabilitation
What should I expect as I recover?
Rehabilitation after anterior lumbar fusion with cages can be a slow process. Although recovery time is different for each paitent, the Family Physiotherapy outpatient physiotherapy program usually begins a minimum of six weeks after surgery. This delay is needed to make sure the fusion is taking. You will probably need to attend physiotherapy sessions for two to three months, and you should expect full recovery to take up to eight months. However, physiotherapy can usually progress faster for patients who had fusion with instrumentation.
At first, our treatments are used to help control your pain and inflammation. Ice and electrical stimulation treatments are commonly used to help with these goals. Our physiotherapist may also use massage and other hands-on techniques to ease muscle spasm and pain.
As you recover, your physiotherapist at Family Physiotherapy will slowly add active treatments, which may include exercises for improving heart and lung function. Short, slow walks are generally safe to start with. Swimming and use of a machine for cardiovascular exercise are helpful in the later phases of treatment. Our physiotherapists also teach specific exercises to help tone and control the muscles that stabilize the low back.
We will also work with you on how to move safely and perform certain activities. This form of treatment, called body mechanics, helps you develop new movement habits. This type of training is designed to keep your back in safe positions as you go about your work and daily activities. Training includes positions you use when sitting, lying, standing, and walking. Our physiotherapist will also help you work on safe body mechanics with lifting, carrying, pushing, and pulling.
As your condition improves, we will tailor your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires strenuous tasks. Our physiotherapist may suggest changes in job tasks that enable you to go back to your previous employer or to do alternate forms of work. We will help you learn to do these tasks in new ways that keep your back safe and free of strain.
Before your physiotherapy sessions end, our physiotherapist will teach you ways to avoid future problems.
Family Physiotherapy provides services for physiotherapy in Edmonton.
Portions of this document copyright MMG, LLC.
